Success Story: Freeman
In January 2016, the Pine Hollow team noticed something seemed off just before driving out of the Winter Equestrian Festival (WEF) with their horses. Stopping to check the horses before continuing off the showgrounds, Pine Hollow discovered Freeman, a promising and successful Dutch Warmblood, had swung his hind leg over the back of the trailer. Freeman’s stifle had ended up squarely on one of the hooks used to secure the back door, lodging the hook into his stifle and into the femoropatellar joint.
Emergency Veterinary Care
Recognizing the extreme peril facing Freeman, Pine Hollow immediately called for help from Palm Beach Equine Clinic, the Official Veterinarians of WEF.
“It took tremendous effort, creative thinking, and exceptional teamwork to free Freeman from the hook impaling his leg,” said David Blake, Pine Hollow’s internationally acclaimed rider and trainer. “Palm Beach Equine Clinic sent several of their top vets to help us rescue Freeman. The team of vets is truly great.”
Thanks in very large part to the help and determination of the vets, Pine Hollow and Palm Beach Equine Clinic were able to free Freeman from the trailer door.
At the Equine Hospital
From there, Freeman was transported to the nearby Equine Hospital, where he spent a few days recovering before it was agreed to pursue arthroscopic surgery on his femoropatellar joint.
“To be honest, it wasn’t looking good at all for the first day or so Freeman was there,” said Blake. “The joint was so severely damaged we didn’t know if it could be fixed. Our only chance of fixing the joint was surgery, so we agreed we would try everything possible.”
Dr. Weston Davis performed the surgery, after which Freeman remained in Palm Beach Equine Clinic’s care while he regained use of the leg.
“The team did a fantastic job there and kept Freeman until he was ready to begin long-term rehab with James Keogh,” said Blake.
When Freeman was finally ready to return home to Pine Hollow, Blake hoped at best Freeman would eventually be able to do light work and perform at a low level.
In the past, when a horse’s gait has felt off or lacking in its usual impulsion, it was often assumed to be an issue of lameness. Now however, thanks to the improved diagnostics readily available at the Palm Beach Equine Clinic veterinarians are able to more accurately pinpoint the problem area. Perhaps surprisingly, it’s not always in the legs or hooves. With increasing frequency, the horse’s neck is being diagnosed as the root of the issue.
The Anatomy of the Equine Neck and What Can Go Wrong
In order to understand the problems that can arise in association with the horse’s neck, it’s important to first understand the anatomy.
The neck is composed of seven cervical vertebrae running from the head to the thorax, named C1 through C7, and each articulating with each other. The primary purposes of the neck are to move the head and to protect and transport the spinal cord and nerves, which run through the middle of the vertebrae.
Such a major role as the protection of the nerves and spinal cord can also come with some major risks and complications, with clinical signs of these problems generally presenting themselves either neurologically, as neck pain, or as lameness in the front legs. These more specific symptoms may include:
- Ataxia or clumsiness – Ataxia is defined as the “lack of control of bodily movements”. In the case of an ataxic horse, you may begin to notice staggering, sudden loss of balance, or even an inability to remain upright. Ataxia is generally an indicator of a neurological condition or damage to the spinal cord itself, caused by either developmental issues, trauma, or an infectious disease such as equine protozoal myeloencephalitis (EPM). Such neurological cases can often be the most debilitating.
- Lameness – You can think of the spinal cord and the nerves in the neck like an interstate, with the spinal cord itself acting as the major highway. As you are “driving” along the interstate, every so often there are little exits, which is where the other nerves come out. Should there be any impingement on the interstate or spinal cord itself, you’re likely looking at more severe complications – much like an accident on the highway. Should there be impingement on the nerves coming off of the spinal cord, it will more likely present itself like an accident a little way off an exit – not affecting the interstate itself, but possibly causing problems that spread elsewhere. That is where we see lameness issues arise.
This can be more difficult to pin down, but can often be due to pressure on the smaller nerves that pass through the openings in the vertebrae and supply the front legs. Arthritis of the articular facet joints of the vertebrae is another common reason for lameness, as anytime these joints become arthritic or inflamed, it can easily translate to the forelimbs.
- Neck Pain – This will often go hand-in-hand with lameness, as factors such as arthritis of the articular facet joints can lead to both symptoms. Other possible reasons for neck pain include trauma or inflammatory diseases.
Diagnosing the Problem
Neck problems, particularly those related to lameness, are generally diagnosed through a process of exclusion, first performing nerve blocks to or ruling out lower regions of the horse’s body. Palpation of the neck, testing of the neck’s movement, and full neurological exams may also be performed in addition to a full lameness exam, depending on the horse’s symptoms.
Once other regions of the horse are ruled out as the location of the problem, veterinarians are now able to use diagnostic images such as radiographs, nuclear scintigraphy and standing CT scans to specifically locate problems in the neck like never before.
In years past, those diagnostic resources were left for last-ditch cases when veterinarians really could not pinpoint any other problems. Today, with the advent of more modern technology, better radiographs, better ultrasound machines, and the more advanced imaging of nuclear scintigraphy and CT scans, veterinarians are able to readily utilize advanced diagnostics to save time and money, and to find the root of the problem more quickly and accurately.
The neck is one of the areas that has most clearly benefited from the progression in advanced imaging. While neck problems have likely been prevalent for some time, veterinarians are now finding those diagnoses more common, as they are able to more accurately locate the issue – particularly at clinics like Palm Beach Equine Clinic. Often these issues will go undiscovered or undiagnosed in the field, but they can be identified at Palm Beach Equine Clinic thanks to the readily available imaging tools.
As an example, if arthritic factors are suspected, nuclear scintigraphy can be used to look for areas of increased bone turnover. On the resulting bone scan, veterinarians are looking for areas where there is an increased calcium uptake because the bone is actively remodeling. These areas will appear darker on the scan and are generally a good indicator of a boney injury or arthritis, with the darker “hot spots” often appearing above the articular facet joints.
Also new and groundbreaking for the diagnosis of equine neck problems is the use of a Computerized Tomography or CT scan, with the ability to scan a standing horse with light sedation on the near horizon which will be available at the clinic this upcoming winter season.
Treatment
Once a solid diagnosis is arrived upon, the proper treatment protocols can be prescribed. Depending on the root of the problem, possible treatments may include shockwave therapy, regenerative therapies such as interleukin-1 receptor antagonist protein (IRAP) therapy or platelet-rich plasma (PRP) therapy, or one of the most common treatments, injections of the facet joints.
In the case of facet joint injections, veterinarians at Palm Beach Equine Clinic are able to medicate under ultrasound guidance, guiding a needle into the joints and delivering corticosteroids or similar medication. Surgery is also an option as a final approach to severe complications.
In milder cases, treatments may also just call for increased time off, chiropractic treatments, or the administration of non-steroidal anti-inflammatory (NSAID) medications.
If you suspect any issues with your horse’s neck, contact Palm Beach Equine Clinic any time by calling (561) 793-1599 to schedule an appointment.
Success Story: Rescue Pony Amazing Grace
On the morning of December 30, 2015, Laurie Waggoner, director of rescue operations and founder of the South Florida SPCA, got a call that she gets all too often. Agriculture patrol had received reports of three emaciated horses in Miami Gardens, FL, that needed immediate care. Waggoner took action and hooked up her truck and trailer to make the drive to pick up the three horses. When she arrived, she found an Arabian and a Quarter Horse, both severely underweight, and a pony she estimated to be two years old laying in the mud, too weak and malnourished to even stand.

The pony, who was quickly named Amazing Grace or “Grace” had been down for more than 24 hours. Despite Waggoner’s best efforts, her team was unable to get Grace on her feet and decided the most humane option was to end Grace’s suffering. Calls went out to local veterinarians, but were met with a slow response the day before New Year’s Eve. While they waited for a veterinarian to become available, Waggoner and her team rolled Grace onto a blanket and carried her onto a trailer to make the trip back to the South Florida SPCA.
“When we pulled her off the trailer, she immediately started grazing,” said Waggoner. “The vet was on the way to euthanize her, but I saw that there was fight still left in her. We were able to pick her up and she stood with help. She was not ready to go.” Grace was made comfortable in a stall at the South Florida SPCA and stood with assistance over the next day. But, on the second day, she was no longer willing or able to make an effort to stand.

“I knew we were going to need help, but it was a holiday and locally everything was closed,” said Waggoner. “I called Palm Beach Equine Clinic (PBEC) and they told me to bring her right in.” Grace arrived at PBEC on New Year’s Day and was greeted by a team of veterinarians led by Dr. Scott Swerdlin, president of PBEC. She was treated for extreme starvation and neglect, which included constant blood work to monitor organ function, the administration of fluids, several meals of senior feed and alfalfa each day, and a lot of compassion from PBEC veterinarians.
Watch Amazing Grace’s Full Story
“She spent eight days at PBEC and returned to the South Florida SPCA ranch with the same will to live,” said Waggoner. “Five days later, I came out in the morning and she was standing on her own.” Grace was completely rehabbed in four months and put up for adoption at the end of 2016. On December 31, 2016, one year after she was found on the brink of death, Grace made her way across the U.S.-Canadian border to her new home at Sherwood Farm in St. Catharines, Ontario, with adopter Marilyn Lee.

“I knew she would need special handling to give her the chance to succeed, which we were fully prepared to do,” said Lee, who also adopted a Thoroughbred from the South Florida SPCA in 2012. “I saw her current photo on South Florida SPCA’s Facebook page and thought, ‘Now there is a lovely pony’. Then I saw the photo of her laying in the dirt, and that was that.” One of Lee’s young riders, Abby Banis, had also learned of Grace’s story on social media and was waiting for the pony in the early morning hours the day she arrived at Sherwood Farm.
The two have been inseparable ever since. Grace’s training began immediately under the direction of Lee’s daughter, Robin Hannah-Carlton. Impressed by the pony’s love for jumping, Lee made plans to start showing Grace. The rescue pony won a reserve championship in the pony hunter division at the very first show she competed in with Banis in the irons.
Today, Grace is happy and healthy with the care of Lee and her staff, and the love of a little girl. The South Florida SPCA operates under the motto, “Your next champion just might be a rescue”, and for Grace, nothing could be closer to the truth.

Read more about Amazing Grace
- South Florida SPCA article “Against All Odds: Rescue Pony Overcomes Abusive Past and Shines in the Show Ring”
- Chronicle of the Horse article “Amazing Grace Went From At-Risk Rescue To Beloved Show Pony”
- The Dodo “‘Lifeless’ Pony Had No Idea How Her Life Was About To Change”
This month, Palm Beach Equine Clinic welcomed a new face to their team. Dr. Katie Atwood, hails from Jacksonville, FL, and attended veterinary school at the University of Florida, making her return to south Florida from Lexington, KY, a special homecoming.

What brought you to Palm Beach Equine Clinic?
I grew up in Florida, so I wanted to be closer to family and the ocean! But, I was also looking for an opportunity to grow and become a better veterinarian. This is a difficult industry to get into, but it is especially difficult to find the right practices. This is a chance for me to work with some of the best doctors in the country.
What would you say is your specialty at Palm Beach Equine Clinic?
In addition to general, preventative and sport medicine, I will be focusing on Palm Beach Equine Clinic’s reproductive work. I did an internship and a fellowship in reproduction and realized that it is what I am most interested in. I will be working on breeding mares, performing frozen and fresh semen inseminations, as well as breeding management and embryo flushes for transfers to recipient mares.
What inspired you to be a veterinarian?
When I was a little kid we had a trail behind our house that was really popular and I would sit on the back wall and watch everybody ride by on their horses. We do not have any other veterinarians in my family, but when I was five years old I realized that I wanted to work with animals. During my undergraduate studies in Animal Science at Berry College in Rome, GA, a professor named Dr. Martin Goldberg really pushed me to pursue veterinary school.
I wake up every morning so excited to go to work and if I don’t come home exhausted and filthy then I have done something wrong. It is an “every minute of every day” commitment, but very rewarding.
When you aren’t working, where can we find you?
I like to spend as much time as possible in the water. I can usually be found swimming, diving or paddleboarding at the beach and spending time by the pool

What advice would you give to someone considering pursuing veterinary school?
Do it! It will be the most difficult time of your life, but if you have a passion for it, it will be so rewarding. Dedication is so important; take advantage of every wet lab you can, go to any conference that is available, and take advantage of opportunities to meet new people and gain mentors. Who wouldn’t want to do what they love for a living?
Name one thing most people wouldn’t know about you?
I am a pretty open book at this point. But, when I retire, my fiancé Mackenzie and I want to sail around the world!
Shes Packin Fame: Back in Winning Form
Nearly eight months ago, Shes Packin Fame, a 2012 Quarter Horse mare owned by Margo Crowther of Fort Myers, FL, suffered a rare slab fracture to the central tarsal bone in her left hock while competing in a barrel racing competition. After a diagnosis aided by Palm Beach Equine Clinic’s (PBEC) state-of-the-art diagnostic imaging equipment and a surgery performed by PBEC’s own Dr. Weston Davis, Shes Packin Fame has not only returned to running barrels, the five-year-old mare is back to winning.

Crowther purchased Shes Packin Fame, affectionately known as Sissy, as a three-year-old after the mare reminded her of a horse she ran in college. Crowther trained Sissy herself and won or placed in nearly every barrel futurity she entered during the horse’s four-year-old year, accumulating $100,000 in prize money.
In November of 2016, Crowther and Sissy were competing at the No Bull Finals in Asheville, NC, when Sissy went down at the first barrel on the final day. The fall fractured the horse’s central tarsal bone, which was not easily diagnosed. Crowther met with a veterinarian in North Carolina who was unable to locate the fracture via x-ray before contacting Dr. Davis, who had managed Sissy’s healthcare since she joined Crowther’s string.
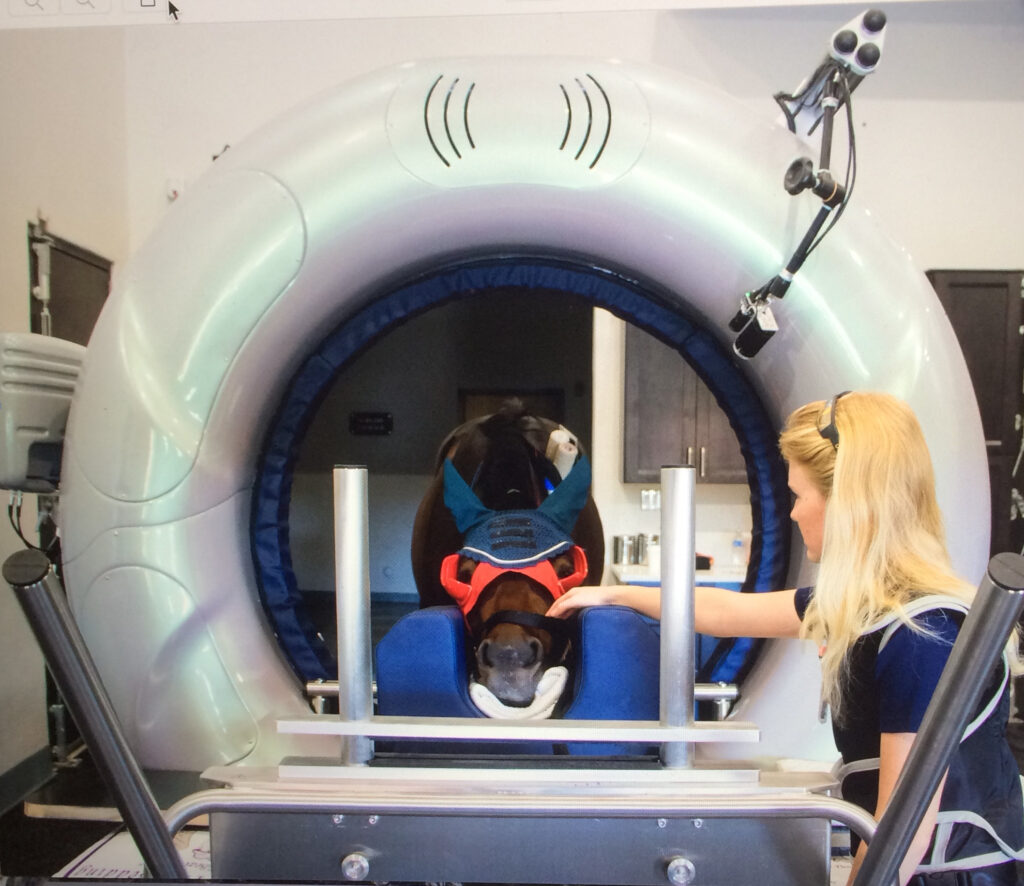
Dr. Davis utilized PBEC’s Equine Standing Magnetic Resonance Imaging (MRI) and Nuclear Scintigraphy (bone scan) modalities to locate a flat piece of separated bone known as a slab fracture.
The process began with a bone scan where Sissy was injected with a radioactive isotope named Technetium 99. The isotope attached to the phosphorous proteins localized within the bone and was absorbed. A specialized nuclear isotope gamma ray camera was used to capture images of the skeletal anatomy with a 360-degree view. Points of interest lit up on the image to indicate increased metabolic activity and was able to locate the site of the injury.
Following the identification of the injured area, a Standing MRI produced highly detailed images in several different planes to capture a compete view of the injury and further define the issue.
After Dr. Davis located and identified the fracture, he surgically inserted a screw into the central tarsal bone to stabilize the fracture. Sissy was discharged from the clinic on six months of recovery with follow-up diagnostic imaging every month to monitor the injury’s repair. During the fourth month of recovery, Dr. Davis removed the screw. At the end of March, Sissy was cleared to begin exercise and Crowther began by hand walking the mare slowly progressing to trotting her under tack. They started with ten minutes of exercise and worked up to 45 minutes.
“Weston was a huge part of Sissy’s recovery,” said Crowther, who set her sights on entering Sissy in the Old Fort Days Derby, held over Memorial Weekend in Fort Smith, AR. “It is the biggest derby of the year for five-year-olds. When it came time to enter, Weston rechecked the leg, did flexion tests, cleared her to run, and wished me good luck.”
When they arrived in Fort Smith, Sissy had not seen a barrel since the day of the injury. Crowther and Sissy posted a time of 16.405 seconds, the fastest time of the event, to win the 25-horse final and collect a $23,469 prize money check.
“She just came back so confident and so strong, like she never missed a beat,” said Crowther. “She always ran like an older horse, but I was surprised at her time. I knew she would be in the top ten, but I was surprised just how strong she was. Weston told me to let her set her own pace and that is what I did. I did not push her. So, when I called Weston to tell him we had won, he was very surprised.
“She feels like her hock is maybe even stronger than it was before the injury,” continued Crowther. “I am so thankful to Weston and Palm Beach Equine Clinic, and feel blessed that she has come back strong and healthy.”
With Sissy back in top form, Crowther’s next goal is a lofty one. Her hope is to qualify for and compete at the National Finals Rodeo in Las Vegas, NV, this December.
Originally hailing from Chicago, Illinois, Brittany Cain attended Southern Illinois University before moving to Florida and joining the staff of Palm Beach Equine Clinic as the manager of the Nuclear Scintigraphy department.

What is your background with horses?
Growing up, my parents actually had nothing to do with horses; we’re from the city of Chicago, so they were not horse people at all. I was just always the horse obsessed little girl – you know, the one horse girl in the class! When I was about 13, I started volunteering at a therapeutic riding center, so I got a lot of hands on experience there. I learned to ride a little bit and worked with the special needs kids. That was great.
When I was 18 years old and had my first paying job, I was able to afford actual riding lessons and it just went from there!
I did a lot of work on Standardbred breeding farms up in Illinois. I foaled out a lot of babies and trained a lot of weanlings. Many of those yearlings went on to be race horses. I did that for three years during college, and that was a really neat experience.
What led you to pursue a career as veterinary technician?
Throughout high school, I was always obsessed with horses. I volunteered all of my free time to be at the barn. I knew I wanted to do something that I loved, so I found Southern Illinois University, and they had a bachelor’s degree in equine science. I applied to one school, got in, and it was perfect. I didn’t have to find a bunch of schools; I just went to the one that I wanted right away, and I knew what I wanted to do!
What led to your focus on the Nuclear Scintigraphy Department in particular?
I’ve always had a strong interest in the anatomy of horses. I knew a lot of equine anatomy from college where I took many courses that covered the musculature anatomy as well as skeletal. In addition, working with all of the Standardbred yearlings was great experience for working with the two and three-year-old racehorse patients that see here at Palm Beach Equine Clinic.

What is your typical day like at Palm Beach Equine Clinic?
As the manager of the Nuclear Scintigraphy Department, I have the patients in the scanning area for bone scans. Myself and technicians will bring the horse into the area, I will take their temperature, pulse, and respiration checks, and then I will place a catheter and inject the radioactive isotopes.
It takes two hours for the isotope to settle into the bones, and then I can begin the bone scan. I usually inject the isotope, and then I do a lot of paperwork in between the two hours since there’s a lot of tracking and recording for dealing with radioactive materials. Then the scan begins. The horse comes into the room; they’re lightly sedated. The scans usually take from one to two hours or, for a full body scan, anywhere from two to four hours. It’s a lot of keeping the horse comfortable, getting all of the images that are needed, and making sure that the images are high quality. Usually during the busy winter season, we have anywhere from two to three horses a day so it keeps me very busy.
What do you enjoy most about working at Palm Beach Equine Clinic?
I love the variety of patients that we see. We get cases of racehorses, polo ponies, barrel racers, top show jumpers, hunters and dressage. It’s really neat seeing all of these talented and often very expensive horses.
Have you had any standout or favorite moments since you joined the Palm Beach Equine Clinic team in 2015?
We went down to Miami for the Longines Global Champions Tour to assist in taking the arriving horses off the airplanes. I helped by taking temperatures, pulse, and respiration checks on all of the competition horses. It was really cool seeing the caravan from the airport to the show grounds and just how it’s set up on Miami Beach.
What do you enjoy doing when you’re not working?
My fiancé and I go fishing a lot usually at the beach or off a pier; we definitely enjoy spending our free time fishing.
Cassidy Hoff is a veterinary technician and assistant to Dr. Richard Wheeler of Palm Beach Equine Clinic. Originally from Middletown, CT, Cassidy joined the team at Palm Beach Equine Clinic in April of 2015.

What is your background with horses?
I’ve always had a passion for horses and I started riding lessons when I was seven years old. I attended Centenary College (now a University) in Hackettstown, NJ, and rode competitively as a student. I graduated in 2012 with a Bachelor of Science in Equine Studies with concentrations in Riding Instruction and Therapeutic Riding Instruction, receiving an additional PATH certification (Professional Association of Therapeutic Horsemanship International).
How did you start at Palm Beach Equine Clinic?
I moved to Florida after graduating from college in 2012 and landed my first job as the head instructor of a therapeutic riding center. I worked there for about three years. Through that experience, I realized that I had a strong interest in the veterinary side of the equine industry. Dr. Greenfield was the center’s primary veterinarian, which is how I learned about Palm Beach Equine Clinic. I applied for a job at Palm Beach Equine Clinic and the timing was perfect to work for Dr. Wheeler.
What is your typical day like?

We usually work six days a week, but during the busy winter season, seven days a week is more likely. Typically, my day begins around 8 a.m. and continues until we are finished with our client appointments. At the end of our day, I send out reports to clients we worked with throughout that day which contain discharge instructions for the findings from each appointment.
Dr. Wheeler mainly focuses on sport horse medicine. I assist him with lameness evaluations, joint injections, ultrasound exams, nerve blocks, and taking radiograph images. I am also responsible for keeping the truck well stocked and organized, replacing medications we use throughout the day and administrative work. Additionally, we complete many pre-purchase exams and I am responsible for putting together the findings for the final exam documents.
What do you like most about your job?
I love the teamwork aspect. A lot of the horses we treat compete in the WEF Saturday Night Lights or in the AGDF Friday Night Stars classes. Being able to watch these top competitions is even more exciting when you know the horse and their whole team! I feel lucky to be working with Palm Beach Equine Clinic and these horses at the top levels of their sport, and even more fortunate that the clients are amazing to work with. It takes a village to get a horse to the top levels and it is really exciting to be a part of that.
What do you do when you are not working?
I still try to find time to ride, which will always be a passion of mine. It is a little bit easier during the off-season summer months. I also enjoy going to the beach, hanging out with friends and reading.
It’s no secret that in nearly any medical condition, early diagnosis can lead to a better prognosis – and colitis in horses is no exception. The inflammation of the colon that defines colitis can be fatal, although fortunately, with the proper detection of symptoms and immediate treatment, a positive outcome and recovery far outweigh a negative ending.
Understanding colitis – the symptoms, diagnostics, and treatment— can help in recognizing the condition. Palm Beach Equine Clinic’s Dr. Selina Watt has helped provide some fundamental information that horse owners and barn managers should be aware of in regards to equine colitis.
Understanding Colitis and Its Causes
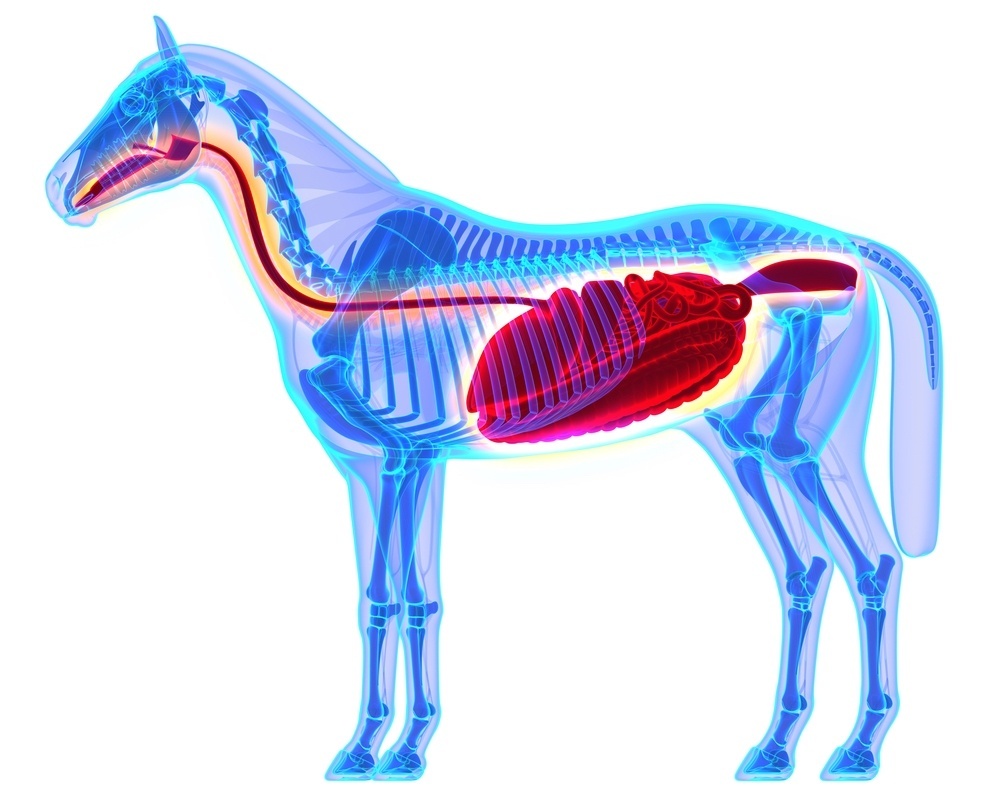
Located in the equine hindgut is the large colon, where microbial digestion and water absorption occurs. The large colon averages 12 feet in length and can hold approximately 20 gallons of feed material and water. When the colon becomes inflamed, the horse is diagnosed with colitis.
While the general definition of colitis is simple and straightforward, the causes can be broader. However, two of the most prevalent causes of colitis are bacterial infections or overuse of medication. Colitis from infectious bacteria is often caused by agents such as Salmonella, Clostridium difficile, or Neorickettsia risticii (Potomac Horse Fever). The non-infectious, right dorsal colitis is often related to the use of non-steroidal anti-inflammatory drugs such as phenylbutazone (Bute).
No matter the cause, each form of colitis leads to a similar inflammation of the large colon. The inflamed colon causes the horse to have diarrhea, as the colon is unable to properly perform its job of adequately absorbing water, electrolytes, and nutrients from the intestinal content. As the condition progresses, leaky membranes of the colon may cause a release of toxins into the bloodstream and the horse will suffer a loss in protein levels. This condition can ultimately affect the entire body as bacteria and toxins circulate, potentially leading to laminitis, founder, protein deficiencies, and a greater risk of complications or lack of a full recovery.

Symptoms and Diagnostics
The first and most conspicuous symptom of colitis is diarrhea. If diarrhea persists, horses can begin to show signs of dehydration and protein loss due to the volume of fluids and nutrients being excreted. Keeping a watchful eye on the consistency of your horse’s manure can be key to catching this condition early. Fever or a lack of energy or appetite may be indicators of colitis and it is recommended to not wait to see what develops but to rather contact a knowledgeable veterinarian for proper diagnostics right away.

Once the horse is under the care of a veterinarian, one of the first things that should be done is bloodwork. In the case of colitis, bloodwork will show decreased white blood cells and protein levels. The severity of the results will indicate how advanced or severe the condition may be. The horse will also generally present with an elevated temperature, and a diagnostic abdominal ultrasound will likely show thickening of the intestinal wall.
Following the initial diagnosis of colitis, a fecal sample is sent to a laboratory where it is tested and analyzed for various forms of bacteria. Comprehensive laboratory results will determine whether the colitis case is infectious or non-infectious. Non-infectious cases can also be diagnosed based on the horse’s history, such as if the horse has been administered Bute for a prolonged period of time.
Treatment and Prognosis
Horses affected by colitis generally require hospital admittance, as they will need fluid therapy and gastro protectants to aid the intestinal wall. If the colitis is caused by infectious bacteria, the patient will also require antibiotic treatment and proper biosecurity measures to prevent transmission. If the bloodwork indicates low protein levels, plasma therapy may also be necessary.
At Palm Beach Equine Clinic, the intensive care management team consists of veterinarians and hospital staff available 24 hours a day, seven days a week. Equine colitis cases cannot simply be administered fluids and left to improve, instead, they require careful monitoring around the clock. If the veterinarian feels the colitis case is severe, the horse may need hourly assessments. This can be of the utmost importance, as colitis cases often rapidly deteriorate without proper veterinary monitoring and swift care.
There is no guaranteed prevention plan for colitis, however, careful management of non-steroidal anti-inflammatory drugs and optimal nutrition can help minimize a horse’s risks of developing the non-infectious colitis condition. With early detection, diagnosis, and proper treatment, equine colitis patients present a positive prognosis.
To ensure the health of your horse, the veterinary team at Palm Beach Equine Clinic is available 24/7. Speak with a Palm Beach Equine Clinic veterinarian regarding the proper medication and nutritional needs of your unique horse by calling 561-793-1599.

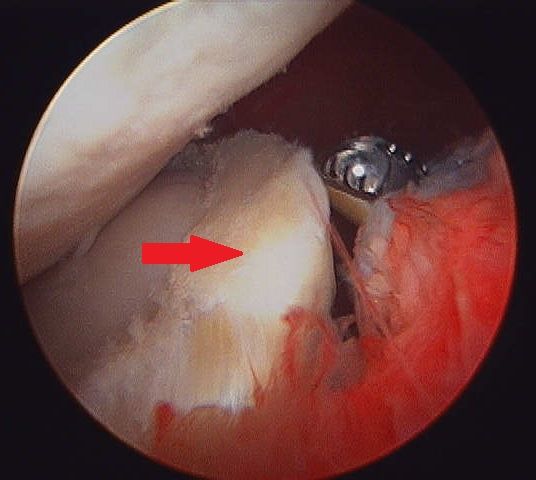
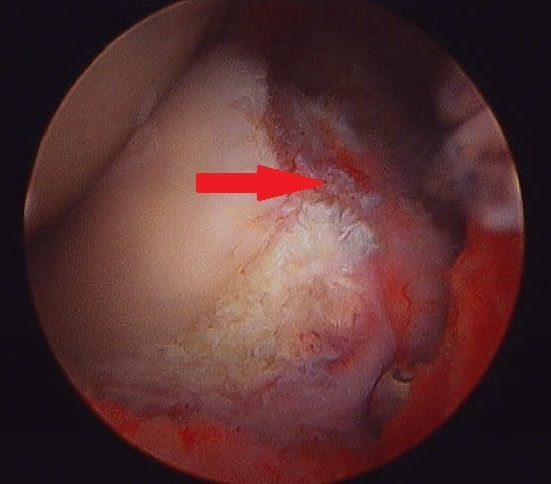
At Palm Beach Equine Clinic in Wellington, FL, the team of Board-Certified surgeons are experts in minimally invasive surgical techniques, aiming to reduce joint disease, resolve lameness, and improve the longevity of sport horse careers.

Arthroscopy (or arthroscopic surgery) is a minimally invasive surgical technique that can be performed on an injured joint or synovial structure to accurately explore and treat pathology. The surgery generally involves two very small (8mm) keyhole incisions. The first incision is where the surgeon will insert the arthroscope, which is an instrument with a small surgical grade camera installed that allows a complete, clear view of the interior joint surface. The second small incision is created to insert the surgical instrument to perform the procedure.
Arthroscopy is used to treat a broad range of injuries inside of a joint. Chip fracture removal is a procedure that is particularly commonly in both young Warmblood horses with developmental disease and in racehorses travelling at high speeds. A small chip fracture can cause persistent irritation in the joint as well as arthritis if left untreated. It is best removed immediately so that no further damage is created. The surgeon can go into the joint, remove the chip, and clean up the surrounding cartilage. Most horses recovery quickly and return to their normal athletic activity.
Board-Certified Surgeon Dr. Weston Davis performs many arthroscopic surgeries at Palm Beach Equine Clinic alongside fellow surgeons Dr. Robert Brusie and Dr. Jorge Gomez.
“In many horses, we consider arthroscopy as a prophylactic measure, intervening after injury, but before the development of a generalized degenerative arthritic cycle ensues,” Dr. Davis stated. “Arthroscopy is definitely something that you want to do early in the game if you feel like the horse has joint disease, or a chip, or cartilage disease, or an undefined injury that is not responding appropriately to medical therapy. Arthroscopy can be curative for some of these horses. But if you do not intervene early on in the course of the disease and there is already advanced arthritis, then you have missed your window.
“Arthroscopy is a preferred treatment because it is minimally invasive so most horses can go right back to work,” Dr. Davis continued. “In a typical scenario, we thoroughly explore the joint with the arthroscopic camera, we remove a chip or repair a lesion, and the horse is not lame after the surgery. Because of the small incisions, there is minimal aftercare and horses are often able to go back to work quickly.”
Other common indications for arthroscopic surgery are meniscal disease in the stifle, subchondral cystic lesions, primary cartilage lesions, and debridement of damaged tendinous/ligamentous tissue (such as deep digital flexor tendon tears in the navicular bursa). The surgeons at Palm Beach Equine Clinic can perform arthroscopy on virtually any joint in the horse. Anything from the Temporomandibular Joint (TMJ) of the head to the navicular bursa within the hoof capsule can be explored and treated with this minimally invasive approach.
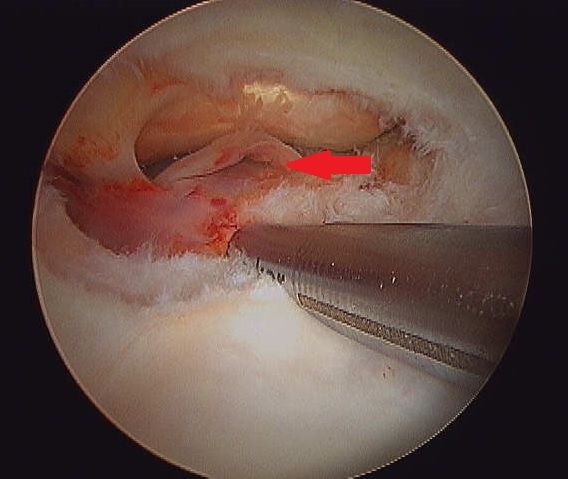

Almost all arthroscopies are performed under general anesthesia with the horse on its back. New renovations at Palm Beach Equine Clinic include a set of stocks of adjustable height adjacent to a surgeon’s pit, allowing the surgeons to have eye-level access to the joint they are working on, enabling many new procedures on the legs of standing horses.
Minimally invasive surgery allows for a simple and quick recovery for the horse. The traditional horse would be on stall rest with a bandage on until the sutures come out at two weeks, and then start doing some light hand walking and physical therapy. Barring severe damage in the joint or associated tendon/ligament disruption, most cases will undergo a six-week rest and rehabilitation protocol, then return to normal work.
As always, the advanced diagnostic imaging at Palm Beach Equine Clinic permits the surgeons to get a complete evaluation of an injury involving a joint to ensure the best possible outcome. Depending on the injury type, digital radiographs, ultrasound, MRI, and Nuclear Scintigraphy, or a combination thereof, may be used for pre-operative diagnosis and planning. Ultrasound and digital radiography are available for intra-operative use. Intra-operative CT scanning will also be available in the future with the new additions at Palm Beach Equine Clinic.
“When you are inside the joint with an arthroscopic camera, you have the most complete picture of the surface and health of that joint,” Dr. Davis noted.
Diarrhea can be a common problem for horse owners, but how do we know when it is serious? What are some of the causes? How do we treat severe cases and what potential complications you should watch for? Internal Medicine Specialist Dr. Peter Heidmann of Palm Beach Equine Clinic in Wellington, FL, has the answers to these questions and more.
Diarrhea, defined as loose stools, or excessive and overly-frequent defecation, occurs when the intestine does not complete absorption of electrolytes and water. Simple changes in feed, exposure to lush grass, or a bite of moldy hay can cause brief irritation of the bowel, giving a horse diarrhea for a day or two, but anything more than that could be from a variety of more serious causes. Bacteria, viruses, and toxins are all factors that can damage the lining of the bowel and lead to equine diarrhea and other complications.
Causes of Equine Diarrhea
The organisms that cause equine diarrhea are mostly bacteria –Salmonella and Clostridium difficile are among the most common. Clostridium difficile is associated with antibiotic use in both people and horses. While antibiotics are useful to kill bad bacteria, they can also kill good bacteria at the same time, upsetting the balance of flora in the body. If a horse goes on antibiotics for any reason, such as a wound or an infection, that can upset the good bacteria in the intestines and cause bad bacteria, such as Clostridium difficile, to grow.
Clostridium difficile can be found naturally in the environment. There are various types of Salmonella, most adapted to birds or to cattle or other livestock, so horses that are around livestock have a higher rate of becoming infected with that particular bacteria. Horses can also carry Salmonella and not have any symptoms, so they can pass it to each other. If the healthy flora in the horse’s body is thrown off by even a small change in diet, or something bigger like a colic episode, or antibiotics, then Salmonella can grow up in its place.
Another bacterial cause of equine diarrhea can be a disease called Potomac Horse Fever. A bacteria called Neorickettsia risticii, which is carried by snails and conveyed by flies like caddis flies, causes Potomac Horse Fever. For this reason, horses that live near rivers or streams can become infected. During warm weather months, caddis flies pick up the bacteria from the streams and can transfer the disease to nearby horses that accidentally eat the flies or larvae. There are hotbeds for Potomac Horse Fever throughout the U.S., including the Potomac basin where it was first described, as well as many parts of the East Coast, and areas of Oregon, northern California, and Montana.

A viral cause of equine diarrhea commonly seen is Coronavirus. This gastrointestinal virus shreds the intestinal lining and can cause horses to become very sick. The body has to reline the bowel, and it does so quickly, but it takes three to five days, during which the horse may have severe diarrhea and secondary infections.
“Coronavirus was thought for a long time to just be an opportunistic infection and that the virus would take advantage of the horse already being sick, but now it is more and more believed to be the cause of its own type of disease,” Dr. Heidmann stated. “Like all of these diseases, it causes damage to the lining of the bowel and supportive care must be used to help the horse heal. Unlike bacterial infections, however, you cannot directly treat the organism, since there aren’t appropriate drugs to directly treat coronavirus in horses.”
Outside of the infectious causes of equine diarrhea, there are mechanical causes, such as ingestion of sand, which can be a common problem in locations like South Florida. Sand is irritating to the lining of the bowel and can cause damage from its weight, as well as its abrasiveness. In general, sand is irritating enough that the body cannot retain the fluid that it needs in the intestines. As a result, it will cause secretory diarrhea where too much water is being lost. Clearing the sand usually solves the problem and the bowel is then able to reestablish a healthy lining.
A final cause of diarrhea in horses is toxins. Toxic plants, such as Oleander, can be fatal in large doses, but if ingested in small amounts, can be a severe irritant to the bowel. Other toxins that a horse can ingest in the environment, such as phosphate or insecticides, may also cause diarrhea.
Treatment for Equine Diarrhea
The single most important treatment for diarrhea, no matter the cause, is supportive care. Supportive care includes providing intravenous fluids to replace the fluids lost, providing protein in the form of plasma for the protein lost due to lack of absorption, as well as balancing electrolytes.

The next most important step is taking measures to either reestablish good flora within the gut or to remove the bad bacteria. In the past, a powdered charcoal was used, which is great for absorbing bacteria, but does not absorb the water. A gastrointestinal health supplement called BioSponge® came on the market in the early 2000s through the company Platinum Performance. The product is a purified clay powder that binds the toxins, and also binds the water, so that the horse loses fewer fluids in their equine diarrhea.
While absorbing the bad bacteria and toxins is important, also providing good bacteria in the form of probiotics can be very helpful.
“Probiotics are very variable in their efficacy, but there are some bacteria that are known to be associated with gut health,” Dr. Heidmann noted. “The good bacteria in people, and in horses, that has the most data for being helpful is Saccharomyces Boulardii. Old-fashioned brewers yeast is also Saccharomyces, but it is a different species, Saccharomyces cerevisiae.
“One of the best ways to re-establish healthy flora is Transfaunation, which is taking a healthy horses manure, filtering it, and then tubing it into the sick horse,” Dr. Heidmann added. “That is one of the most dramatic treatments out there. It provides the good ‘bugs’ that the horse is losing through the diarrhea. You will often see foals eating their mother’s manure. It is an instinctual habit to get the good bugs into their stomach. We only do that in the sickest of cases. Whatever the route, it makes a big difference to provide the good bugs because that creates the environment for the gut to heal.”
While some antibiotics are warranted in the right situation, Dr. Heidmann pointed out that they are not necessary as often as people would think.
“With people or dogs, if we get Salmonella or some other intestinal infection, we almost always go on antibiotics, but because antibiotics are the cause of many cases of colitis in horses, in general, that is not the best strategy,” Dr. Heidmann stated. “There are a couple of exceptions. Clostridium difficile does respond to antibiotics, metronidazole being the most common one. For Potomac Horse Fever, Tetracycline broad-spectrum antibiotics are the best.”
Biosecurity measures should also be taken to protect healthy horses from an infectious barn-mate. Dr. Heidmann recommends complete isolation of the sick horse while it is ill, and for a minimum of two full weeks after the infection has been clinically resolved. This includes no horse-to-horse contact, as well as no shared use of wheelbarrows, pitchforks, etc.
Molecular and DNA testing can be done to make sure that the horse is infection-free, however, Dr. Heidmann warns that testing can be problematic.
“There is a very high number of false negatives, meaning there is truly some infection there, but the lab cannot find it,” Dr. Heidmann stated. “There can be times when the horse is shedding bugs, but the tests do not pick it up. The state-of-the-art standard of care is a DNA test called ‘PCR’, and yet you still have to do multiple tests to get a positive test and get a diagnosis. Still, the best way to be safe is to continue testing until you are sure.”
Complications of Equine Diarrhea
Dr. Heidmann warned of common complications in severe diarrhea cases, laminitis being highest on the list. With the sickest of horses, it is unfortunately not uncommon for the veterinarian to get the gut fixed over three to five days, and then find that the feet have started to become very inflamed due to toxins in the bloodstream. If the horse loses the lining of its intestine, then the good and bad bacteria that are supposed to be contained in the intestine can “leak” out into the bloodstream and are free in the abdomen. Those bacteria are then dying either from an attack by the immune system or antibiotics, and they release endotoxins into the bloodstream, which along with other inflammatory products, can cause laminitis.
Another serious complication is blood clotting. The sick horse may become very low on blood protein when the bowel lining is damaged, which can cause clotting abnormalities. The horse may have difficulty clotting or they may become prone to abnormal increases in clotting. The horse might seem better, and then it will develop a clot somewhere in the body. It can be anywhere, but it is most often in the intestine itself, which is usually fatal. In general, horses like this are treated with supplemental protein in the form of plasma. In some cases, the veterinarian will also provide anticoagulant medications.

Although some cases of equine diarrhea are brief and easily resolved, Dr. Heidmann reminds that serious cases can go downhill fast, and it is important to refer to an expert.
“The biggest sign of a problem is duration,” Dr. Heidmann concluded. “If it is one day, it could be that they had a bite of bad food or something simple. If there are fevers or lethargy, those are instant warning signs. If it lasts for days, or if they go off their feed, those are instant warning signs. That is when you should call your veterinarian right away, especially because as they start to go downhill, these complications really amplify. The worst cases are the ones that have been smoldering for a day or two.”
Dr. Heidmann and the veterinarians at Palm Beach Equine Clinic are always available and encourage owners to contact the clinic at the first sign of a problem.


